Managing Skin Picking(Dermatillomania)
How To Stop Skin Picking
If you’re reading this, you’ve probably already tried to stop skin picking. Many times. Maybe you’ve made it a few days, or even a few weeks, before finding yourself back at the mirror. If that sounds familiar, you’re in the right place.
Here’s the honest answer upfront: there’s no cure for skin picking. No single technique that makes the urge disappear. But there are a lot of things that genuinely help, and for most people, the right combination leads to real, lasting improvement.
That word “combination” matters. Skin picking is driven by a tangle of habits, emotions, triggers, and brain wiring. Managing it usually means addressing several of those things at once. What works for one person won’t work for another, and that’s normal. The goal isn’t to find the one perfect solution, it’s to build a toolkit that works for you specifically.
This page covers everything we currently know about what helps: from techniques you can try right now, to professional therapies with strong research behind them, to practical skin care and the harder stuff like shame and talking to someone about it.
Want to know where to start? Take our test to get personalized recommendations based on your specific picking patterns.
Self-Help Strategies for Skin Picking
You don’t need a therapist to start making progress. These techniques are evidence-informed and practical and things you can try on your own, starting today.
Awareness Training
The first step isn’t stopping. It’s noticing.
A significant amount of skin picking happens automatically (i.e. your hand is on your face before your brain catches up). Awareness training is about closing that gap. Not eliminating the urge, but learning to catch it earlier so you have a window to make a different choice.
A few ways to build this:
Name it when it happens. When you notice you’re picking or about to pick, say to yourself — even just in your head “I’m picking” or “my hand is moving.” It sounds almost too simple, but naming the behavior shifts your brain out of autopilot and into conscious awareness. That’s where change starts.
Track your episodes. Logging when you pick, even a quick note of the time, what you were doing, and how you were feeling, builds a pattern map over time. You’ll start to see which situations and emotional states are your biggest triggers. That information is genuinely useful.
Use physical cues. Some people wear a textured ring, put bandaids on their fingertips, or keep a rubber band on their wrist, not to snap it, but as a physical reminder to check in. When your fingers feel different, your brain notices.
The point isn’t to judge yourself every time it happens. It’s to shrink the gap between “I’m picking” and “I noticed I’m picking.” That gap is where change happens.
Competing Responses
A competing response is a physical action that makes picking impossible because your hands are occupied doing something else. The concept comes from habit reversal training (more on that below), but you can use it on your own right now.
When you notice the urge, or catch yourself mid-pick, replace it with a different action. The key is choosing something genuinely incompatible with picking. Some options:
- Clench your fists and hold for 30 seconds
- Press your hands flat against your thighs or a desk
- Cross your arms
- Pick up a fidget toy or stress ball
- Put your hands in your pockets
- Hold something cold
It doesn’t matter much which one you use. What matters is consistency and doing it every time the urge hits. Over time, the new response starts to become as automatic as the picking was.
Fidget Tools and Sensory Substitutes
A lot of skin picking is driven by a need for tactile stimulation. Your fingers want something to do, and your skin is right there. Giving them an alternative isn’t willpower, it’s meeting the same sensory need through something that doesn’t cause damage.
The best fidget tools for skin picking have textures or resistance that mimic what fingers are looking for: something to pick at, peel, press, or manipulate. Popular options include textured fidget rings, spiky sensory balls, peel-off nail polish or craft glue (for the peeling sensation), putty or clay, pop-it toys, and textured picking stones.
The placement rule is non-negotiable: keep them where you actually pick. Next to the TV, on your nightstand, on your desk, in the bathroom. If the alternative isn’t within arm’s reach when the urge hits, it won’t help.
Barrier Methods
Sometimes the most effective thing is simply putting something physical between your fingers and your skin. Barriers don’t address the underlying urge, but they slow you down and protect healing skin.
Options worth trying: hydrocolloid patches or bandaids over sites you frequently pick, gloves or finger covers during high-risk times like watching TV or lying in bed, long sleeves if you pick at your arms, keeping nails very short, or tape on fingertips to change the sensation enough to disrupt automatic picking.
Barriers work best as part of a broader approach rather than the only strategy. Used alone, most people eventually work around them. Used in combination, they can meaningfully reduce damage.
Environment Changes
If you can change the environment where picking happens, you can reduce how often it happens. This is about making picking less convenient and less automatic, not through sheer willpower, but by changing the physical setup.
Start with mirrors. If you pick in the bathroom, try dimming the lighting, covering part of the mirror with a frosted film, or setting a timer before you go in. A lot of people find that removing magnifying mirrors alone makes a noticeable difference. Some people put a sticky note on the mirror that says something simple like “be kind to your skin.” It sounds small, but interrupting the automatic routine is exactly the point.
Adjust lighting. Bright, close-up lighting makes it easy to spot the imperfections your brain wants to “fix.” Softer lighting removes some of that visual pull.
Manage high-risk times. If you pick while watching TV, have a fidget tool on the couch. If you pick scrolling your phone, try holding the phone in a different position or wearing a ring that keeps your fingers occupied. If bedtime is a danger zone, consider lightweight gloves.
Small environmental shifts can have outsized effects because they break the automatic chain of events that leads to picking, before you even have to resist anything.
Habit Tracking
Tracking your picking can feel uncomfortable at first. Nobody wants to keep a log of something they wish they weren’t doing. But it’s one of the most powerful tools available because it converts a vague, shame-heavy experience into concrete, usable information.
When you track consistently, you start seeing patterns that would otherwise be invisible. Maybe you pick most on Sunday evenings. Maybe it spikes before a particular kind of conversation. Maybe it’s worse the week before your period. These aren’t random, they’re patterns, and patterns can be planned for.
What to log: when you picked, how long it lasted, what you were doing beforehand, how you were feeling, where on your body, and what (if anything) helped you stop. A notebook, spreadsheet, or a dedicated app all work — the format matters far less than the consistency.
Therapeutic Approaches for Skin Picking
Self-help strategies can take you a significant way. But sometimes you need more structured support. These are the therapeutic approaches with the strongest evidence behind them for skin picking disorder.
Cognitive Behavioral Therapy
CBT is the most widely recommended treatment for skin picking disorder, and it has the most robust research behind it. The version used for skin picking focuses on the relationship between your thoughts, feelings, and picking behavior.
In practice, CBT for skin picking involves identifying the thoughts and beliefs driving your picking (“I need to make this smooth” or “I can’t focus until I fix this spot”), learning to challenge those thoughts, developing alternative coping responses, and practicing them over time. Treatment is typically 8–12 sessions with a psychologist or therapist, though some people benefit from longer work.
One important caveat: CBT requires active participation between sessions. The homework is where most of the change happens. This isn’t a passive “show up and get fixed” process, but that effort is also exactly why it works.
Habit Reversal Training (HRT)
HRT is often delivered as part of CBT, but it deserves a standalone mention because it’s one of the most reliably effective techniques for skin picking specifically.
It has three core components:
Awareness training: Systematically mapping when picking happens, what triggers it, and what the early warning signs look like (the urge, the hand movement, the mirror-scanning behavior). This is the same concept from the self-help section, but done more rigorously in a therapeutic setting.
Competing response training: Identifying a specific physical action to perform when the urge hits, and practicing it until it becomes reflexive. Your therapist helps you find something that works for your particular patterns.
Social support: Optionally involving a partner, friend, or family member who can gently flag picking behavior and encourage the competing response. Not everyone uses this component, but it can meaningfully accelerate progress.
Research consistently shows HRT is among the most effective treatments for BFRBs. Improvement usually takes weeks of consistent practice, not days, but it does come.
Acceptance and Commitment Therapy (ACT)
ACT takes a different angle. Rather than trying to control or eliminate urges, it teaches you to accept them without acting on them.
The core insight: you can have the urge to pick and still choose not to. The urge itself isn’t the problem, it’s what you do with it. ACT uses mindfulness techniques, values clarification, and “cognitive defusion” (learning to observe your thoughts without being driven by them) to help you build a fundamentally different relationship with the picking impulse.
Many people find ACT useful because it removes the framing of failure. Feeling the urge isn’t the problem. You’re not losing, you’re practicing. And the more you practice sitting with the urge without acting on it, the less hold it has over time.
ACT is often combined with HRT for skin picking, and that combination has solid research support. If willpower-focused approaches have left you feeling like you’re fundamentally broken, ACT is worth exploring.
Comprehensive Behavioral Treatment (ComB)
ComB is a treatment model designed specifically for BFRBs like skin picking. Rather than a single technique, it’s a framework that tailors intervention to your individual picking profile.
The model identifies five types of cues that maintain picking: sensory, cognitive, affective (emotional), motor (physical habits), and place/setting. ComB starts by figuring out which cues are most prominent for you, then targets those specifically.
If your picking is primarily triggered by the texture of a bump (sensory), treatment focuses on sensory substitutes. If it’s driven by perfectionist thoughts about your skin (cognitive), the emphasis shifts to challenging those beliefs. Most people have a mix, so treatment typically addresses several cue types at once.
ComB is newer than CBT and HRT, but early evidence is promising, and many BFRB specialists use it in practice because of how well it accounts for individual differences.
Finding a Therapist
Here’s something nobody tells you upfront: finding a therapist who actually knows skin picking is harder than it should be. Many general therapists haven’t trained in BFRBs and may not know the techniques that work. Seeing one of them can sometimes feel frustrating and unproductive.
What to look for: experience with BFRBs or OCD-spectrum conditions specifically, training in HRT, CBT for BFRBs, or the ComB model. The TLC Foundation for BFRBs maintains a therapist directory that’s a good starting point. And telehealth has genuinely changed the options here, you’re no longer limited to whoever practices in your city.
Ask directly when contacting potential therapists: “Have you treated skin picking disorder before? What approach do you use?” A therapist who answers honestly is more valuable than one who says yes to everything.
Medication for Skin Picking
This section is informational, not medical advice. Medication decisions should always be made with a doctor who knows your full picture. That said, here’s what the research currently shows.
SSRIs
Selective serotonin reuptake inhibitors (SSRIs), the same class of medications used for depression and anxiety, are the most studied medication option for skin picking disorder. The evidence is mixed but cautiously positive.
Some studies show SSRIs reduce picking urges and frequency; others show minimal benefit over placebo. The general clinical consensus is that SSRIs can help some people, particularly when picking is accompanied by significant anxiety or depression. They tend to work better as part of a combined approach, medication alongside therapy, than alone.
Commonly studied SSRIs for skin picking include fluoxetine (Prozac), sertraline (Zoloft), and escitalopram (Lexapro). If you’re considering this route, a psychiatrist is typically better placed to prescribe and monitor than a general practitioner.
NAC (N-Acetylcysteine)
NAC is an over-the-counter supplement that’s generated real interest in the BFRB community. It’s an amino acid that affects glutamate signaling in the brain, a system thought to play a role in compulsive behavior.
A notable clinical study found NAC significantly reduced skin picking in a portion of participants, and it has a much more favorable side-effect profile than most prescription options.
The evidence base is still relatively small, and it doesn’t work for everyone. It’s not a substitute for behavioral strategies, but some people find it takes the edge off urges, making other techniques easier to actually use. Talk to your doctor before starting it; “over-the-counter” doesn’t mean zero interactions or considerations.
Other Medications
Researchers have also looked at antipsychotics, glutamate modulators, and opioid antagonists, but the evidence for these in skin picking is limited and side-effect profiles are more significant. They’re generally only considered when other approaches haven’t worked.
The overall picture on medication: it can be a useful piece of the puzzle for some people, but it’s rarely the whole answer. The strongest outcomes consistently come from combining medication with behavioral therapy.
Skin Care After Picking
This section isn’t about prevention, it’s about what to do after a picking episode to help your skin heal and minimize scarring. Because self-criticism doesn’t speed up healing, but proper wound care does.
Immediate Aftercare
Right after picking, the goal is simple: clean, protect, leave it alone.
Clean gently. Wash the area with lukewarm water and a mild cleanser. Skip anything alcohol-based, heavily fragranced, or astringent – irritated skin doesn’t need more aggravation.
Apply an occlusive product. Vaseline, Aquaphor, or a dedicated wound-healing ointment creates a moisture barrier that actively speeds healing. The “let it air out” instinct is outdated and research consistently shows moist wound healing is faster and produces less scarring.
Cover it. Hydrocolloid patches (the kind designed for blisters or acne) are a genuine game changer. They protect the wound, keep it moist, absorb fluid, and, importantly, create a physical barrier that makes it harder to re-pick the same spot. They also conceal the damage, which can help short-circuit the shame spiral that sometimes triggers more picking.
Leave scabs alone. Every time a healing wound gets reopened, it restarts the inflammation process and increases scarring risk. Keeping it covered helps with this more than willpower alone.
Scar Management
If you have scarring from skin picking, you’re not alone, and there are real options. Addressing visible scarring can also support recovery by reducing one of the main sources of shame that keeps the cycle going.
For newer dark marks (post-inflammatory hyperpigmentation): Vitamin C serums, niacinamide, and alpha hydroxy acids like glycolic acid can help fade discoloration over time. Consistent sunscreen is essential and UV exposure makes dark marks significantly worse and prevents them from fading.
For older or raised scars: Silicone scar sheets and gels have solid evidence for flattening and fading raised scarring. Chemical peels (glycolic, salicylic, or TCA) can improve texture. For deeper or more significant scarring, professional options like microneedling, laser therapy, or subcision are worth discussing with a dermatologist.
Be honest with yourself about timelines. Post-inflammatory marks can take 3–12 months to fade, and scars may take longer. Starting the right routine now means meaningful improvement ahead, just not immediately.
One important note: for some people, skin care routines can actually trigger picking, anything involving close mirror time, examining texture, or touching the face. If that’s you, keep your routine fast and minimal. Get in, do the basics, get out. The most sophisticated routine in the world isn’t worth a 45-minute picking session.
Dealing With Shame and Telling Someone
Skin picking disorder thrives in silence. Most people who have it carry it entirely alone, hiding marks, making excuses, canceling plans when the damage feels too visible. The shame often becomes as hard to live with as the picking itself.
If you’ve never told anyone, you’re not unusual. You’re in the majority. But carrying it alone has real costs: it reinforces the idea that this is something to be ashamed of, it cuts off potential support, and it makes the whole thing feel heavier and more permanent than it needs to be.
Telling someone doesn’t have to be a big revelation. It can be as simple as: “I want to tell you about something I deal with. I have something called dermatillomania, I compulsively pick at my skin. It’s a recognized condition, and I’m working on it. I just wanted you to know.”
That’s genuinely enough. You don’t owe anyone a detailed explanation or a look at your skin. You decide how much to share and with whom.
Who to tell first? Whoever feels safest. For most people, that’s a close friend rather than a partner or family member, someone who tends to listen without immediately jumping to solutions.
What if they don’t understand? Some people won’t. A lot of people have never heard of skin picking disorder, and some will say things like “just stop touching your face”, frustrating, but usually coming from ignorance rather than indifference. You can share resources (like this site) or simply let them know you’re not looking for solutions, just acknowledgment.
Talking to a doctor. Most doctors don’t ask about BFRBs, so you’ll likely need to raise it yourself. A direct approach works well: “I compulsively pick at my skin and I haven’t been able to stop. It’s affecting my life and I’d like to discuss treatment options.” If your doctor seems unfamiliar with the condition, ask for a referral to someone who specializes in OCD-spectrum disorders or BFRBs.
Apps and Tools for Skin Picking
Technology isn’t a replacement for the strategies above, but it can make them significantly easier to actually maintain.
What to Look For
The most useful apps for skin picking tend to include episode tracking (logging when you pick, your triggers, and your emotional state), pattern recognition (surfacing trends and high-risk situations from your data), guided activities (breathing exercises, competing response reminders, mindfulness), and progress monitoring (showing how things are changing over time, because it’s genuinely difficult to perceive gradual improvement from inside the experience).
The best tool is the one you’ll actually use. A feature-rich app you open once isn’t helping anyone. Look for something that fits naturally into your day and doesn’t make you feel worse about yourself when you log an episode.
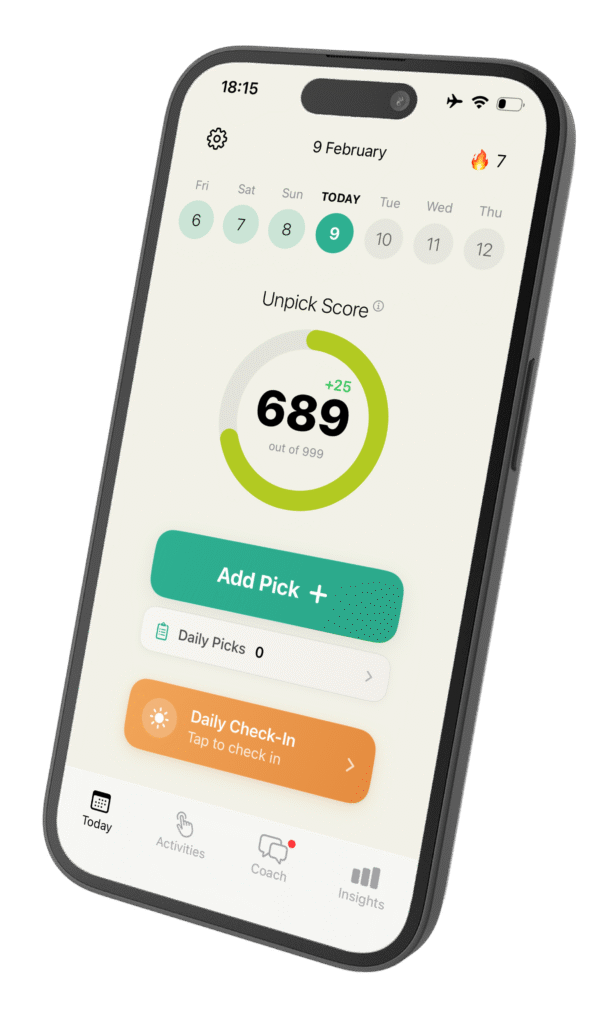
Unpick
Unpick is an app we built specifically for skin picking. It was designed around the evidence-based approaches on this page, awareness training, episode tracking, pattern recognition, and guided activities — brought together in one place.
Here’s what it does:
Episode tracking — log picking episodes quickly, with details about triggers, emotions, and location. Designed to be fast and non-judgmental so you’ll actually do it consistently, not just when things are going well.
Pattern recognition — the app analyzes your tracking data and surfaces trends you might not spot yourself: which days are hardest, what emotional states appear most, which situations are highest risk.
AI coaching — personalized guidance based on your specific patterns, with real-time suggestions and support when you need them.
Guided activities — exercises grounded in CBT and mindfulness for use in the moment when urges hit, or as a daily practice.
Progress monitoring — track how your picking is changing over time through your Unpick Score, so you can recognize improvement even on days that feel hard.
It won’t cure anything overnight, and it’s not a substitute for therapy if therapy is what you need. But it puts proven tools in your pocket for the moments between sessions, or when you’re not ready for a therapist yet.
Building Your Approach
There’s no single right way to manage skin picking. What works is personal, and it usually takes some experimentation. But most people find it helpful to work through roughly this sequence:
Start with awareness. Before trying to change anything, spend a week or two just observing when, where, and why you pick. Don’t judge it. Just gather data. What you learn will tell you where to focus.
Add one or two self-help techniques. Based on your patterns, choose strategies that target your biggest triggers. If you’re a mirror picker, start with environment changes. If it’s mostly automatic picking during downtime, start with fidget tools and competing responses. Trying to overhaul everything at once leads to burnout, start small and build.
Consider therapy if self-help isn’t enough. If you’ve been working consistently for a couple of months without meaningful progress, or if your picking is severe, professional support can make a significant difference. Seek out someone trained specifically in BFRBs.
Discuss medication if it’s relevant. Especially if anxiety or depression is fueling your picking, the right medication can provide enough relief to make behavioral strategies actually land. This is worth an honest conversation with a doctor.
Track your progress. Gradual improvement is genuinely hard to perceive from the inside. Tracking gives you objective data that can sustain motivation when it feels like nothing is changing.
Expect setbacks. Reducing skin picking is not a straight line. Bad days don’t erase good weeks. The people who make lasting progress aren’t the ones who never slip — they’re the ones who keep going after they do.
Frequently Asked Questions
How do I stop picking my skin?
There’s no instant fix, but a combination of strategies works for most people. Start with awareness training and fidget tools, use competing responses when urges hit, and consider therapy, especially habit reversal training or CBT, if self-help isn’t enough. Building a toolkit matched to your specific triggers is more effective than searching for one universal solution.
What is the best therapy for skin picking?
Cognitive behavioral therapy (CBT) with habit reversal training (HRT) has the strongest evidence for skin picking disorder. Acceptance and commitment therapy (ACT) is also effective, particularly when combined with HRT. Look specifically for a therapist with experience treating BFRBs, not just general anxiety or OCD.
Can you manage skin picking without therapy?
Yes, many people see real improvement through self-help strategies alone. Awareness training, competing responses, fidget tools, environment changes, and consistent tracking can all make a meaningful difference. Therapy becomes most valuable when self-help alone isn’t enough or when picking is severe.
Do fidget toys actually help with skin picking?
They can, particularly for people whose picking is driven by a need for sensory stimulation. Fidget tools give your hands an alternative to satisfy that need. They work best when kept within reach during high-risk moments, watching TV, lying in bed, sitting at a desk, not stored away somewhere.
What medication helps with skin picking?
SSRIs are the most studied medication for skin picking disorder, with mixed but cautiously positive results. NAC (N-acetylcysteine), an over-the-counter supplement, has shown promise in some studies. Medication tends to work best alongside behavioral therapy rather than as a standalone treatment. Always discuss options with a doctor.
How do I heal my skin after picking?
Clean the area gently with a mild cleanser, apply an occlusive product like Vaseline or Aquaphor, and cover with a hydrocolloid patch. For existing scarring, options include silicone scar sheets, vitamin C serum, and professional treatments like microneedling. Consistent sunscreen is essential to prevent dark marks from worsening.
How long does it take to reduce skin picking?
It varies significantly. Some people notice improvement within weeks of consistent effort; for others it takes months. Skin picking disorder tends to be chronic, with periods of improvement and occasional setbacks. The goal is steady, meaningful progress over time, not overnight perfection.
Take the Next Step
You don’t have to do everything on this page at once. Start with one thing that resonated, try it for a couple of weeks, and build from there.
Take our test and answer a few quick questions about your picking patterns, with personalized recommendations for where to start.
Download Unpick for evidence-based tracking, AI coaching, and guided activities in your pocket.
Read Understanding Skin Picking to learn more about what skin picking is, what causes it, and how it connects to conditions like anxiety and OCD.